Fortnightly Prostate Cancer News
New Biopsy Grades and Screening Tests. Improved therapies.Screening and Grading - Replacing Gleason 3+4=4+3
Toward a new prostate cancer grading system — step 1The basic premise is that all prostate cancers can be subdivided, histopathologically, into five categories described in the table below:
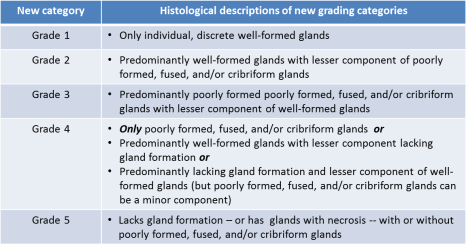
there are three important points that we will all need to understand as we start to adapt to this new prostate cancer grading system:
- It gets rid of all the inherent complications of the existence of the Gleason scores from 1 + 1 = 2 to 3 + 2 = 5, none of which are currently reported any more anyway, but whose existence prejudices everyone’s thinking because the lowest reported Gleason score today is 3 + 3 = 6.
- It deals effectively with the fact that Gleason 3 + 4 = 7 really is a different form of histology compared to Gleason 4 + 3 = 7.
- It differentiates between cancers that are more like Gleason 4 + 4 = 8 and those that are more like Gleason 9s and 10s.
Don't eliminate PSA without Replacing PSA
PSA screening rates: 2005 to 2013 | THE "NEW" PROSTATE CANCER INFOLINKAn article by Drazer et al., now available in the Journal of Clinical Oncology, and presented a few weeks ago at the annual meeting of the American Society of Clinical Oncology in Chicago, is based on data from the nationally representative National Health Interview Survey. (This paper is also discussed in an article on the Medscape web site.) Prostate cancer screening significantly declined among men older than age 50 years after the 2012 USPSTF guideline discouraging PSA-based screening. A significant proportion of men continue to be screened despite a high risk of 9-year mortality, including one third of men age 75 years and older.
The problem we continue to be faced with is that the PSA test is a very poor indicator of real risk for clinically significant prostate cancer. Yes, it is true, it is what we had at the time. But arguably there are two better tests available now (the Prostate Health Index or phi test and the 4KScore test). And what we really need is some clarity about how best to use those tests in making determinations about who to biopsy, and about whether one of those tests really is better than the other or not.
It is also worth noting that, based only on the Choosing Wisely initiative, several organizations are now very clear that PSA-based screening for risk of prostate cancer is inappropriate in men with a life expectancy of < 10 years (regardless of the patient’s calendar age).
Helping Doctors and Patients make Wise Choices
New recommendations from the AUA through “Choosing Wisely” initiativeThe complete list of 10 recommendations issued by the AUA through the Choosing Wisely initiative can also be found on line. Previously the AUA had advised its members and other clinicians that, with respect to risk for prostate cancer:
- Don’t treat an elevated PSA with antibiotics for patients not experiencing other symptoms.
- A routine bone scan is unnecessary in men with low-risk prostate cancer.
- Don’t recommend screening for … prostate cancer if life expectancy is expected to be less than 10 years (AMDA).
- Don’t routinely perform PSA-based screening for prostate cancer (American College of Preventive Medicine).
- Don’t recommend screening for … prostate … cancer without considering life expectancy and the risks of testing, overdiagnosis and overtreatment (American Geriatrics Society).
- Don’t perform PSA testing for prostate cancer screening in men with no symptoms of the disease when they are expected to live less than 10 years (American Society of Clinical Oncology).
- Don’t routinely screen for prostate cancer using a prostate-specific antigen (PSA) test or digital rectal exam (American Academy of Family Physicians).
- Don’t routinely recommend proton beam therapy for prostate cancer outside of a prospective clinical trial or registry (American Society for Radiation Oncology).
- Don’t initiate management of low-risk prostate cancer without discussing active surveillance (American Society for Radiation Oncology).
- Don’t perform PET, CT, and radionuclide bone scans in the staging of early prostate cancer at low risk for metastasis (American Society of Clinical Oncology).
Effects of Diet
Prostate cancer: risk of death may be raised by Western diet - Medical News TodayThe researchers found that those who ate a predominantly Western diet (those in the highest quartile) were two-and-a-half times more likely to die from prostate cancer and had a 67% increased risk of all-cause mortality compared with participants in the lowest quartile. In comparison, the men who follow a "prudent" diet closely had a 36% lower risk of all-cause mortality.
The researchers noted a number of other characteristics concerning the followers of the two particular diets. Those who scored highest for the "prudent" diet consumed less animal fat and alcohol and were more likely to have never smoked. Men scoring highest for the Western diet tended to be older at prostate cancer diagnosis and had lower intakes of calcium and vitamin D.
Radiation Therapy
“Dose painting” — a new type of radiation therapy for prostate cancer?Two technologies have been brought together to allow for a new kind of radiation treatment known as simultaneous integrated boost (SIB) or, more informally, “dose painting.” The two technologies are:
- Improved imaging by PET scans and multiparametric MRIs, for example, that can more precisely locate tumors within the prostate, and
- Improved external beam technology that can deliver doses with submillimeter accuracy.
- Is there any benefit in terms of oncological outcomes?
- Is there any increase in treatment toxicity attributable to it?
Odds for PCa Recurrence and Mortality after EBRT
Risk factors for primary radiation failure and timing of progressionThe Natural History and Predictors of Outcome Following Biochemical Relapse in the Dose Escalation Era for Prostate Cancer Patients Undergoing Definitive External Beam Radiotherapy - European Urology
The researchers found that:
- 23 percent of patients experienced biochemical failure.
- The median time from biochemical failure to detection of distant metastases was 5.4 years.
- The median time from biochemical failure to prostate cancer-specific mortality was 10.5 years, 5.1 years after metastases were detected.
- Risk of clinical progression following biochemical failure were independently associated with:
- Shorter PSA doubling time
- Higher clinical stage
- Higher Gleason score
- Shorter time to biochemical failure
Radiation and ADT Therapy Improves Results for PCa
Combining ADT and salvage radiation therapy improves outcomes | THE "NEW" PROSTATE CANCER INFOLINKChemo Therapy
Docetaxel with radiation in prostate cancer treatmentBenefits of adding Chemo for Advanced PCaAbstract #5001 & #LBA5002 - Highlights from the Genitourinary (Prostate) Cancer Oral Abstract Session | ASCO Annual Meeting
Next Big Future: Improved combination treatment against high-risk, localized prostate cancer
Two abstracts presented during the Genitourinary (Prostate) Cancer Oral Abstract Session on Sunday, May 31, showed significantly improved overall survival (OS) when docetaxel chemotherapy was added to standard hormone therapy in patients with advanced, hormone-naive prostate cancer (Abstract 5001) and hormone therapy plus radiation therapy in men with high-risk localized prostate cancer (Abstract LBA5002)
STAMPEDE
Nicholas D. James, MD, PhD, of the University of Warwick and Queen Elizabeth Hospital Birmingham, United Kingdom, presented the first OS results from the randomized, controlled STAMPEDE trial, a multistage, multi-arm assessment of therapies for men with advanced, hormone-naive prostate cancer.Arm deaths median OS
SOC plus docetaxel arm 165 77 months
SOC alone arm 405 67 months .
RTOG 0521
Howard M. Sandler, MD, of Cedars-Sinai Medical Center, presented the results of the phase III RTOG 0521 trial, a federally funded trial that compared outcomes in 562 men with high-risk, localized prostate cancer treated with androgen suppression and radiation therapy with or without the addition of adjuvant chemotherapy with docetaxel and prednisone.After a median of 6 years follow-up,
Arm deaths 4-year OS
SOC docetaxel/prednisone chemotherapy 36 93%
SOC Radiation/ADT standard therapy 52 89%
Genetics
CRPC, “personalized” medicine, and the science of whack a moleWe have known for decades that prostate cancer is an “evolutionary” cancer. In other words, clinically significant prostate cancer and prostate cancer-specific mortality are the consequence of a series of events over time (probably both genetic and epigenetic) that lead to progressive and then to metastatic disease of variable levels of aggression.
What we do not know yet is exactly how and why prostate cancers are initiated; what events are necessary to make a prostate cancer tumor sufficiently aggressive to start to spread through and outside of the prostate; exactly why some prostate cancers are more aggressive than others; etc.; etc. On the other hand, what we have been discovering over the past decade is that literally hundreds of mutations to cancer cells may be associated with the progression of prostate cancer over time. Some of these are common and are probably “necessary” to the development of clinically significant disease. Others are much less common and we have no real idea yet just how important they may be in the development of clinically significant prostate cancer — indeed, they may be an effect of the disease progression as opposed to a cause.
8 comments:
The information is really helpful to me. First time I am reading this article and found accurate relevant information. Thanks for sharing such a useful information. Calcium is the major component of our bones know
The information is really helpful to me. First time I am reading this article and found accurate relevant information. Thanks for sharing such useful information. Calcium is the major component of our bones know calcium requirements and its natural resources
The information is really helpful to me. First time I am reading this article and found accurate relevant information. Thanks for sharing such a useful information. Calcium is the major component of our bones know calcium requirements and its natural resources
I find this information incredibly helpful! It's my first time reading this article, and I've come across some very accurate and relevant details. Thank you for sharing such valuable insights! Fmovies
nice information i like this article visit our site for free movies and tvshows Hurawatch
if you want Chandelier cleaning service visit our site Chandelier cleaning service
Post a Comment