Prostate Cancer News 07-24-2015
Prostate cancer: treatment options | CPD article | Pharmaceutical Journal
Treatment of early stage prostate cancer and locally advanced disease
can involve surveillance, radical treatment or androgen deprivation
therapy; however, as the disease progresses, these options change.
Although
patients may require definitive therapy as their disease progresses,
active surveillance is an important treatment option.
Radical
prostatectomy or radical radiotherapy are recommended for men with
intermediate- and high-risk localised prostate cancer, where there is a
prospect of long-term disease control. However, both options are
associated with complications, including impaired sexual function.
Androgen
deprivation therapy has been the mainstay for advanced prostate cancer
management; however, recently there has been a move towards initiating
hormonal treatment in younger men with early disease or recurrent
disease after definitive treatment.
Advanced disease, or
metastatic castrate resistant prostate cancer, usually occurs 12–18
months after diagnosis and androgen ablation, with a median survival of
two to three years. Treatment usually involves chemotherapy with
docetaxel, but a number of newer drugs, including cabazitaxel,
abiraterone and enzalutamide, are available.
General
After years of overtreatment for patients with low-risk prostate cancer,
rates of active surveillance/ watchful waiting increased sharply in
2010 through 2013, and high-risk disease was more often treated
appropriately with potentially curative local treatment rather than
androgen deprivation alone, according to a study in the July 7 issue of JAMA.
Among men 75 years or older, the rate of surveillance was 54 percent
from 1990 through 1994, declined to 22 percent from 2000 through 2004,
and increased to 76 percent from 2010 through 2013. There was an
increase in the use of surgery for men 75 years or older with low-risk
cancer to 9.5 percent and intermediate-risk cancer to 15 percent;
however, there was not an increase in use for those with high-risk
cancer, among whom androgen deprivation still accounted for 67 percent
of treatment.
Understanding the U.S. News Rankings for Prostate Cancer Care? - Cancer Answers
On Tuesday, U.S. News & World Report released its
2015–16 Best Hospitals rankings.
The University of Texas MD Anderson Cancer Center in Houston regained
the No. 1 ranking in cancer care. But does that mean it’s where prostate
cancer patients should go?
As someone who lives with prostate cancer and heads a prostate cancer
nonprofit, I believe the prostate cancer community would benefit from
knowing about this top-ranked hospital’s prostate cancer care. But its
No. 1 ranking doesn’t answer many questions.
What you can do
UnitedHealthcare steps to help prevent prostate cancer:
-
Eat Less Red Meat and Processed Meat. Red meat and processed meats
like bacon have been linked to increased risk of prostate cancer.
- Eat more fruits and vegetables.
- Exercise more and maintain a healthy weight
This pilot randomized dose–comparison trial provides preliminary data to
suggest that RT 3 days per week compared with 2 days per week may
improve the strength and physical functioning in prostate cancer
survivors, but may also blunt improvements in psychosocial functioning.
Larger and more targeted phase II and III trials are needed to confirm
the potentially complex effects of RT frequency in prostate cancer
survivors.
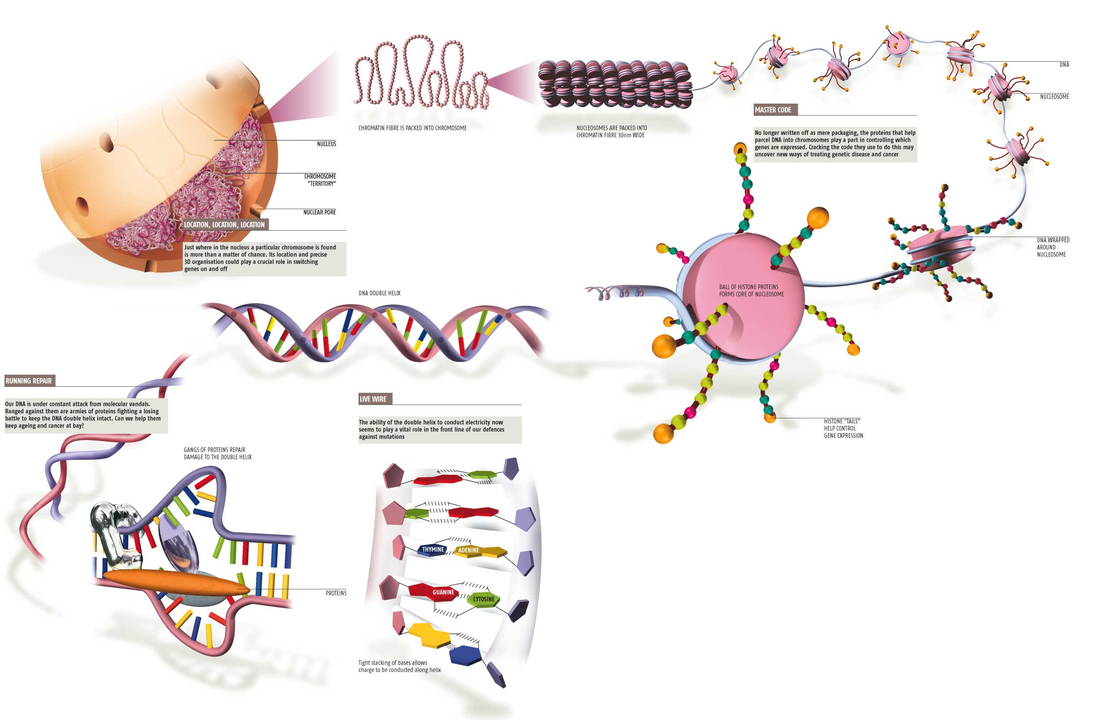
The results of the study were encouraging. The researchers found
that DNA damage decreased as adherence to the modified Mediterranean
diet increased and there was an inverse association between olive oil
intake and DNA damage. On the other hand, DNA damage was reported to
increase with increased consumption of dairy products and red meat.
The
authors also found that higher levels of whole blood monounsaturated
fatty acids and oleic acid were associated with decreased DNA damage,
while high levels of omega-6 polyunsaturated fatty acids were associated
with increased DNA damage.
The benefits of the modified
Mediterranean diet extended to include weight loss and a feeling of
general well-being at the end of the three-month period by some
subjects.
Overall results indicate that changing the Western
dietary pattern to a modified Mediterranean dietary pattern that
includes fish and olive oil can be beneficial in decreasing DNA damage
in men with prostate cancer.
A
review of research on the use of testosterone replacement therapy in
men with a history of prostate cancer and in men with elevated prostate
cancer risk found no evidence of statistically significant associations
between such treatment and cancer progression.
The finding supports the conclusion of several other recent studies that
have attempted to evaluate replacement therapy in such populations and
failed to find evidence of danger. - See more at:
http://www.hcplive.com/medical-news/testosterone-replacement-therapy-and-prostate-cancer-risk#sthash.nr7HYohy.dpuf
A
review of research on the use of testosterone replacement therapy in men with a
history of prostate cancer and in men with elevated prostate cancer risk found
no evidence of statistically significant associations between such treatment
and cancer progression.
The finding supports the conclusion of several other recent studies that have
attempted to evaluate replacement therapy in such populations and failed to
find evidence of danger.
Screening;
Diagnosis
Intermediate and high-risk prostate cancers have seen a major drop in U.S. diagnoses,
according to a recent study led by Vanderbilt University Medical Center, published last month in The Journal of Urology. Don’t be deceived: This is anything but good news.
This significant drop
in the number of diagnoses of intermediate (28%) and high-risk (23%)
prostate cancers is most likely an indication that many of these cancers
are not being found.
John Julius Hungwe (68), a survivor of prostate cancer, said the
condition severely impacts the family. Things were quite difficult in
Zimbabwe as the cost of cancer treatment is quite costly there. Hungwe
said he never wanted to die, as life is so much fun for him.
New
research has shown how a smart sensor chip, able to pick up on subtle
differences in glycoprotein molecules, can improve the accuracy and efficiency
of prostate cancer diagnosis.
Initial
July 6, 2015
Rather than use the historical arbitrary cutoff of a 4.0 PSA
reading to define abnormal, we now have tools to adjust our interpretation of
readings for age (PSA levels normally rise with age); for race (this, too,
affects what is considered normal); and for the size of a man’s prostate, which
affects how much PSA he produces. We can test for how fast PSA levels rise over
time. And we can analyze how PSA circulates in the bloodstream (free or bound
to serum proteins), which can predict prostate cancer risk.
When we use these markers together, these varied
interpretations of PSA levels give us a clearer picture of who does, or
doesn’t, need further testing. And we keep refining our approach. Already, a
urine test can find and measure the presence of genes associated with prostate
cancer. M.R.I. images can
help identify high-risk prostate lesions. And tests for the presence or
activity, or both, of genes present in prostate tissue can help distinguish
which patients can safely defer therapy from those who cannot.
what frustrates urologists most: Rather than using refined
screening techniques to identify those who will benefit most from treatment,
we’re just evaluating fewer men. So the task force needs to re-evaluate its
recommendation based on the current state of medical knowledge.
But men should not wait for a government agency to tell them
what’s best. My own strongest recommendation is that men insist on a baseline
PSA test while in their 40s. From this baseline, a personalized screening
regimen that considers risk factors and other indicators can be developed.
Men must understand that screening does not commit them to
further testing or treatment, even if abnormalities are found. Screening,
followed up with today’s sophisticated tools, simply provides information that
helps them and their doctors make sound decisions — which could prolong their
lives, or leave them reassured that they have little to fear
from an indolent tumor
So long as we go on re-fighting the PSA screening wars, we are not going
to make any significant progress toward a better way to assess risk for
prostate cancer. The PSA test is what it is — an indicator of the
potential for any one of several types of prostate/urinary tract
problem. And that is all it is. Getting an annual PSA test — and
especially getting an annual PSA test while simultaneously refusing to
have a digital rectal examination — is not a way to manage risk for
prostate cancer. On the other hand, not
getting a PSA test when you need one (for all sort of possible reasons)
is about as smart as not getting a vaccination against measles or
tetanus or a whole bunch of other deadly disorders. You may well not
need that vaccination. And you may well find you did not need the PSA
test (just as you may never need certain types of vaccination) … but
under the right conditions, any of these actions might help to save your
life.
The National Cancer Institute (NCI) announced that it had removed all
prostate specific antigen (PSA) data from the SEER (Surveillance,
Epidemiology and End Results) and SEER-Medicare programmes. The PSA data were removed after quality control checks revealed that a
substantial number of PSA values included in the programmes were
incorrect.
The U.S. Preventive Services Task Force (USPSTF) issued a grade D recommendation that discouraged PSA-based screening for prostate cancer in October 2011, according to study background.
“The results raise concern that if this trend continues, more men may be diagnosed at a point when their disease
is advanced,” Barocas said. “Younger, healthier men with intermediate-
or high-risk disease would normally be candidates for aggressive local
therapy and they may not be receiving a timely diagnosis under this
policy.”
Researchers at Sanford-Burnham Medical Research Institute in Orlando are
working to more accurately diagnose prostate cancer starting with a set
of RNA molecules believed to regulate cell development.
Doctor
Ranjan Perera, Associate Professor at Sanford-Burnham Medical Research
Institute, said, "We were able to identify some of these RNAs being
secreted in the urine of the prostate cancer patients." The team
examined the urine and tissue samples of prostate cancer patients with
those who did not have cancer and found the RNA levels were higher in
those with cancer. Researchers say the RNAs are easily detected in
urine.
"Our hope is that we can develop a urine test that would be a better biomarker for diagnosing prostate cancer," said Dr. Patel.
New
screening that could be faster, more accurate, and end up saving even
more lives. Professor Perera says the next step is to initiate a
wide-scale clinical trial. He believes that the clinical study will be
completed and a urine test will be developed and ready for use in three
to five years.
Watching
'Genuine Change' in US
Prostate Cancer Management
In the years 2010-2013, the use of active surveillance for low-risk
disease "increased sharply" to 40% of all cases, say investigators. The
rate had languished at only about 10% in the preceding 20 years.
At
the same time, use of androgen deprivation as a monotherapy "decreased
sharply," they note, down to only 3.8% of intermediate-risk and 24% of
high-risk prostate cancer cases. These percentages represent drops of
about one third and one half from earlier periods.
Both trends are desirable because they represent strategies to avoid overtreatment and undertreatment, respectively.
More
men with prostate cancer are opting for surveillance | Reuters
There are several possible treatments
for prostate cancer, including surgery and radiation. Some men -
especially those who are older - may opt for active surveillance.
Men using active surveillance may undergo tests or biopsies to make sure the cancer isn't growing, the ACS says.
The
approach helps avoid more aggressive treatments, which can carry the
risk for complications such as incontinence and impotence.
Simply
observing men with very low-and low-risk prostate cancer very effective and
underused, UCLA researchers find - Medical News Today
"Ultimately, the decision-making process surrounding treatment for a man
with localized prostate cancer must take an individualized approach.
The risks and benefits of expectant management vis-a-vis active
treatment should be reviewed with the patient in light of existing
knowledge, potentially with the use of decision aids to help enable a
truly shared decision-making process," the review states. "Active
surveillance is a viable approach for most men with low-risk prostate
cancer, and its broader adoption has the potential to stop the
overtreatment of men with indolent lesions and redirect resources to men
with more serious cancers."
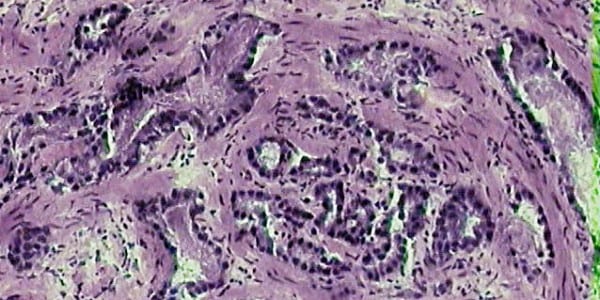
Biopsy/Pathology
Genomics
British
Journal of Cancer - The genomic evolution of human prostate cancer
Prostate cancers are highly prevalent in the developed world, with
inheritable risk contributing appreciably to tumour development. Genomic
heterogeneity within individual prostate glands and between patients
derives predominantly from structural variants and copy-number
aberrations. Subtypes of prostate cancers are being delineated through
the increasing use of next-generation sequencing, but these subtypes are
yet to be used to guide the prognosis or therapeutic strategy. Herein,
we review our current knowledge of the mutational landscape of human
prostate cancer, describing what is known of the common mutations
underpinning its development. We evaluate recurrent prostate-specific
mutations prior to discussing the mutational events that are shared both
in prostate cancer and across multiple cancer types. From these data,
we construct a putative overview of the genomic evolution of human
prostate cancer.
New
Study Published on Cover of Urology Finds that Decipher® Prostate Cancer... --
SAN DIEGO, July 14, 2015 /PRNewswire/ --
The
Decipher test used in this study has been previously described in
multiple blinded independent validation studies in men at high risk of
recurrence at the time of prostatectomy. Researchers found that 60% of
the clinically high-risk men would be reclassified as low risk based on
the Decipher test and have only a 2.4% risk of metastasis at 5 years
after surgery. In addition, the 19% of the patients with the highest
risk based on Decipher had a nearly 10-fold higher risk of distant
metastases by 5 years. The test provided a more accurate and precise
estimate of a patient's risk of recurrence. Use of this test therefore
has the potential to assist clinicians to better direct utilization of
secondary therapy after surgery.
Access
: Which, when and why|[quest]| Rational use of tissue-based molecular testing
in localized prostate cancer : Prostate Cancer and Prostatic Diseases
An increased molecular understanding of localized prostate cancer and
the improved ability for molecular testing of pathologic tissue has led
to the development of multiple clinical assays. Here we review the
relevant molecular biology of localized prostate cancer, currently
available tissue-based tests and describe which is best supported for
use in various clinical scenarios. Literature regarding testing of human
prostate cancer tissue with Ki-67, PTEN (by immunohistochemistry (IHC)
or fluroescence in situ hybridization (FISH)), ProMark, Prolaris,
OncotypeDX Prostate and Decipher was reviewed to allow for generation of
expert opinions. At diagnosis, evaluation of PTEN status, use of
ProMark or OncotypeDX Prostate in men with Gleason 6 or 3+4=7
disease may help guide the use of active surveillance. For men with
Gleason 7 or above disease considering watchful waiting, Ki-67 and
Prolaris add independent prognostic information. For those men who have
undergone prostatectomy and have adverse pathology, Decipher testing may
aid in the decision to undergo adjuvant radiation. Newly available
molecular tests bring opportunities to improve decision making for men
with localized prostate cancer. A review of the currently available data
suggests clinical scenarios for which each of these tests may have the
greatest utility.
Imaging
Dr.
Aaron Ward is designing a road map - a computerized, 3D road map -
to help better diagnose and treat prostate cancer. And it's getting
national attention. A computerized road map uses artificial intelligence
to help interpret the nuances in what's shown through an MRI.
Ward explains that the computer takes three different images of the
prostate with different information, "and the idea is that this
artificially intelligence system is going to automatically integrate and
combine all of this information to produce a much simpler to read
colour-coded road map for where the threatening areas of potential
cancer are."
The
typical biopsy that doctors perform to check a man for prostate cancer is far
from a precise procedure, says the trial’s principle investigator Clare Tempany,
a radiologist and director of the National
Center for Image Guided Therapy at Brigham. Typically a physician
targets the prostate, which is the size of “a small peach or plum,” she says,
by placing a grid guide between the patient’s legs. Then the doctor inserts
needles through the skin and into each quadrant to get tissue samples.
“This is somewhat disparagingly called ‘the blind biopsy,’ ” says Tempany.
“There’s no lesion targeted, it’s just: ‘Let’s push a bunch of needles in and
see what we get.’ ”
These biopsies are sometimes aided by ultrasound
imaging, which requires inserting a ultrasound wand into the patient’s
rectum. Because ultrasound doesn’t provide clear enough images,
doctors aren’t able to make precision strikes with their needles, says
Tempany. They often end up taking 10 to 50 core samples, she says, and each
needle stick carries the risk of infection.
This clinical trial literally shows a better
way. Looking at real-time MRI images, the doctor can identify parts of the
prostate that look suspicious, and direct the robotic tool to those spots.
“In our procedure, a small little robot places the needle on the skin’s surface
and says, ‘This is the spot where you need to push, and in five or six centimeters
you’ll hit your target,’ ” Tempany explains. In the current trial the doctor
takes the actual step of inserting the needle, and typically takes
samples in just four locations. “It’s a smarter biopsy,” she says.
Treatment
Case
Studies Offer Window Into Evolving Prostate Cancer Paradigm
In
the ever-evolving treatment landscape in metastatic prostate cancer,
healthcare providers have more options that ever before. Although
guideline organizations have now incorporated the results of major
clinical trials into treatment paradigms, much controversy remains over
how best to sequence therapies, according to experts who participated in
a recent OncLive Peer Exchange.
In recognition of this complexity, moderator Raoul S. Concepcion, MD, FACS,
and colleagues took a case-based approach to explore the ways in which
oncologists and urologists can employ newly acquired evidence to manage
patients whom they encounter in their practices. The Peer Exchange
session, entitled “Integrating Prostate Cancer Trial Findings Into
Practice: A Case-Based Discussion,” incorporated four cases, two of
which are presented here.
- See more at:
http://www.onclive.com/publications/Oncology-live/2015/July-2015/case-studies-offer-window-into-evolving-prostate-cancer-paradigm#sthash.FozlFACb.dpuf
In the ever-evolving treatment landscape in metastatic prostate cancer, healthcare providers have more options that ever before. Although guideline organizations have now incorporated the results of major clinical trials into treatment paradigms, much controversy remains over how best to sequence therapies, according to experts who participated in a recent OncLive Peer Exchange.
In recognition of this complexity, moderator Raoul S. Concepcion, MD, FACS, and colleagues took a case-based approach to explore the ways in which oncologists and urologists can employ newly acquired evidence to manage patients whom they encounter in their practices. The Peer Exchange session, entitled “Integrating Prostate Cancer Trial Findings Into Practice: A Case-Based Discussion,” incorporated four cases, two of which are presented here.
- See more at: http://www.onclive.com/publications/Oncology-live/2015/July-2015/case-studies-offer-window-into-evolving-prostate-cancer-paradigm#sthash.FozlFACb.dpuf
Radiation
Increased
radiation offers no survival benefit for patients with low-risk prostate cancer
Increased radiation dose is associated with higher survival rates in men
with medium- and high-risk prostate cancer, but not men with low-risk
prostate cancer, according to a new study from Penn Medicine published
this week in JAMA Oncology. Already-high survival rates for men
with low-risk prostate cancer were unaffected by higher radiation
dosages compared to lower radiation dosages.
Hormone Therapy
Androgen
deprivation of prostate cancer: Leading to a therapeutic dead end.
In this review, we describe molecular alterations in tumor cells during
ADT, which lead to deregulation of different signaling pathways and
castration-resistance, and how they might interfere with the clinical
outcome of different second-line therapeutics. A recent breakthrough
finding that early chemotherapy is associated with a significant
survival benefit in metastatic hormone-sensitive disease highlights the
fact that there is time for a fundamental paradigm shift in the
treatment of advanced prostate cancer. Therapeutic intervention seems to
be indicated before a castration-resistant stage is reached to improve
therapeutic outcome and to reduce undesirable side effects.
Chemo
Predicting
response to chemotherapy for prostate cancer and other stories . . . | The BMJ
A new study shows that the measurement of androgen receptor
splice variant 7 (AR-V7) in circulating tumour cells can predict which
men with castration resistant prostate cancer are most likely to respond
to treatment with chemotherapy rather than enzalutamide or abiraterone
(JAMA Oncology 2015, doi:10.1001/jamaoncol.2015.1341).
Detection
of AR-V7 in CTCs from men with metastatic CRPC is not associated with
primary resistance to taxane chemotherapy. In AR-V7–positive men,
taxanes appear to be more efficacious than enzalutamide or abiraterone
therapy, whereas in AR-V7–negative men, taxanes and enzalutamide or
abiraterone may have comparable efficacy. Circulating tumor cell–based
AR-V7 detection may serve as a treatment selection biomarker in CRPC.
Advanced -
Recurrent
A
bird's eye view of advanced prostate cancer
An estimated 220,000 American men are diagnosed with prostate cancer
each year, with 30,000 expected to die of it this year. While androgen
deprivation therapy (ADT) is initially effective against metastatic
disease, most men develop tumors that ultimately become resistant to
ADT, including the most recent ADT regimen (abiraterone acetate and
enzalutamide). This condition is known as metastatic
castration-resistant prostate cancer (mCRPC). While many studies have
cataloged somatic alterations in primary prostate cancers, genomic
studies of mCRPC have been limited to either autopsy samples or
preclinical models. To address the gap in our understanding of mCRPC, an
international and multi-institutional consortium that included Fred
Hutch investigators and benefitted from key contributions from Dr. Pete
Nelson’s Laboratory (Human Biology, Clinical Research and Public Health
Sciences Divisions), sequenced the DNA and RNA from biopsies of bone or
soft tissue metastases prospectively from 150 mCRPC affected
individuals. This work was recently published in the journal Cell.