Prostate Cancer News 07-24-2015
 |
| Study Supports Surgery for High-Risk Prostate Cancer - Renal and Urology News |
Treatment of early stage prostate cancer and locally advanced disease can involve surveillance, radical treatment or androgen deprivation therapy; however, as the disease progresses, these options change. Although patients may require definitive therapy as their disease progresses, active surveillance is an important treatment option.
Radical prostatectomy or radical radiotherapy are recommended for men with intermediate- and high-risk localised prostate cancer, where there is a prospect of long-term disease control. However, both options are associated with complications, including impaired sexual function.
Androgen deprivation therapy has been the mainstay for advanced prostate cancer management; however, recently there has been a move towards initiating hormonal treatment in younger men with early disease or recurrent disease after definitive treatment. Advanced disease, or metastatic castrate resistant prostate cancer, usually occurs 12–18 months after diagnosis and androgen ablation, with a median survival of two to three years. Treatment usually involves chemotherapy with docetaxel, but a number of newer drugs, including cabazitaxel, abiraterone and enzalutamide, are available.
General
After years of overtreatment for patients with low-risk prostate cancer,
rates of active surveillance/ watchful waiting increased sharply in
2010 through 2013, and high-risk disease was more often treated
appropriately with potentially curative local treatment rather than
androgen deprivation alone, according to a study in the July 7 issue of JAMA.
Among men 75 years or older, the rate of surveillance was 54 percent
from 1990 through 1994, declined to 22 percent from 2000 through 2004,
and increased to 76 percent from 2010 through 2013. There was an
increase in the use of surgery for men 75 years or older with low-risk
cancer to 9.5 percent and intermediate-risk cancer to 15 percent;
however, there was not an increase in use for those with high-risk
cancer, among whom androgen deprivation still accounted for 67 percent
of treatment.
Understanding the U.S. News Rankings for Prostate Cancer Care? - Cancer Answers
On Tuesday, U.S. News & World Report released its 2015–16 Best Hospitals rankings. The University of Texas MD Anderson Cancer Center in Houston regained the No. 1 ranking in cancer care. But does that mean it’s where prostate cancer patients should go?
As someone who lives with prostate cancer and heads a prostate cancer nonprofit, I believe the prostate cancer community would benefit from knowing about this top-ranked hospital’s prostate cancer care. But its No. 1 ranking doesn’t answer many questions.
Understanding the U.S. News Rankings for Prostate Cancer Care? - Cancer Answers
On Tuesday, U.S. News & World Report released its 2015–16 Best Hospitals rankings. The University of Texas MD Anderson Cancer Center in Houston regained the No. 1 ranking in cancer care. But does that mean it’s where prostate cancer patients should go?
As someone who lives with prostate cancer and heads a prostate cancer nonprofit, I believe the prostate cancer community would benefit from knowing about this top-ranked hospital’s prostate cancer care. But its No. 1 ranking doesn’t answer many questions.
What you can do
UnitedHealthcare steps to help prevent prostate cancer:- Eat Less Red Meat and Processed Meat. Red meat and processed meats like bacon have been linked to increased risk of prostate cancer.
- Eat more fruits and vegetables.
- Exercise more and maintain a healthy weight
This pilot randomized dose–comparison trial provides preliminary data to
suggest that RT 3 days per week compared with 2 days per week may
improve the strength and physical functioning in prostate cancer
survivors, but may also blunt improvements in psychosocial functioning.
Larger and more targeted phase II and III trials are needed to confirm
the potentially complex effects of RT frequency in prostate cancer
survivors.
The authors also found that higher levels of whole blood monounsaturated fatty acids and oleic acid were associated with decreased DNA damage, while high levels of omega-6 polyunsaturated fatty acids were associated with increased DNA damage.
The benefits of the modified Mediterranean diet extended to include weight loss and a feeling of general well-being at the end of the three-month period by some subjects.
Overall results indicate that changing the Western dietary pattern to a modified Mediterranean dietary pattern that includes fish and olive oil can be beneficial in decreasing DNA damage in men with prostate cancer.
A
review of research on the use of testosterone replacement therapy in
men with a history of prostate cancer and in men with elevated prostate
cancer risk found no evidence of statistically significant associations
between such treatment and cancer progression.
The finding supports the conclusion of several other recent studies that have attempted to evaluate replacement therapy in such populations and failed to find evidence of danger. - See more at: http://www.hcplive.com/medical-news/testosterone-replacement-therapy-and-prostate-cancer-risk#sthash.nr7HYohy.dpuf
The finding supports the conclusion of several other recent studies that have attempted to evaluate replacement therapy in such populations and failed to find evidence of danger. - See more at: http://www.hcplive.com/medical-news/testosterone-replacement-therapy-and-prostate-cancer-risk#sthash.nr7HYohy.dpuf
A
review of research on the use of testosterone replacement therapy in men with a
history of prostate cancer and in men with elevated prostate cancer risk found
no evidence of statistically significant associations between such treatment
and cancer progression.
The finding supports the conclusion of several other recent studies that have attempted to evaluate replacement therapy in such populations and failed to find evidence of danger.
The finding supports the conclusion of several other recent studies that have attempted to evaluate replacement therapy in such populations and failed to find evidence of danger.
Screening; Diagnosis
Intermediate and high-risk prostate cancers have seen a major drop in U.S. diagnoses, according to a recent study led by Vanderbilt University Medical Center, published last month in The Journal of Urology. Don’t be deceived: This is anything but good news. This significant drop in the number of diagnoses of intermediate (28%) and high-risk (23%) prostate cancers is most likely an indication that many of these cancers are not being found.
John Julius Hungwe (68), a survivor of prostate cancer, said the
condition severely impacts the family. Things were quite difficult in
Zimbabwe as the cost of cancer treatment is quite costly there. Hungwe
said he never wanted to die, as life is so much fun for him.
New research has shown
how a smart sensor chip, able to pick up on subtle differences in
glycoprotein molecules, can improve the accuracy and efficiency of
prostate cancer diagnosis.
Read more at: http://phys.org/news/2015-07-sensor-technology-accuracy-prostate-cancer.html#jCp
Read more at: http://phys.org/news/2015-07-sensor-technology-accuracy-prostate-cancer.html#jCp
New
research has shown how a smart sensor chip, able to pick up on subtle
differences in glycoprotein molecules, can improve the accuracy and efficiency
of prostate cancer diagnosis.
Initial
July 6, 2015
Rather than use the historical arbitrary cutoff of a 4.0 PSA
reading to define abnormal, we now have tools to adjust our interpretation of
readings for age (PSA levels normally rise with age); for race (this, too,
affects what is considered normal); and for the size of a man’s prostate, which
affects how much PSA he produces. We can test for how fast PSA levels rise over
time. And we can analyze how PSA circulates in the bloodstream (free or bound
to serum proteins), which can predict prostate cancer risk.
When we use these markers together, these varied
interpretations of PSA levels give us a clearer picture of who does, or
doesn’t, need further testing. And we keep refining our approach. Already, a
urine test can find and measure the presence of genes associated with prostate
cancer. M.R.I. images can
help identify high-risk prostate lesions. And tests for the presence or
activity, or both, of genes present in prostate tissue can help distinguish
which patients can safely defer therapy from those who cannot.
what frustrates urologists most: Rather than using refined
screening techniques to identify those who will benefit most from treatment,
we’re just evaluating fewer men. So the task force needs to re-evaluate its
recommendation based on the current state of medical knowledge.
But men should not wait for a government agency to tell them
what’s best. My own strongest recommendation is that men insist on a baseline
PSA test while in their 40s. From this baseline, a personalized screening
regimen that considers risk factors and other indicators can be developed.
Men must understand that screening does not commit them to
further testing or treatment, even if abnormalities are found. Screening,
followed up with today’s sophisticated tools, simply provides information that
helps them and their doctors make sound decisions — which could prolong their
lives, or leave them reassured that they have little to fear
from an indolent tumor
So long as we go on re-fighting the PSA screening wars, we are not going
to make any significant progress toward a better way to assess risk for
prostate cancer. The PSA test is what it is — an indicator of the
potential for any one of several types of prostate/urinary tract
problem. And that is all it is. Getting an annual PSA test — and
especially getting an annual PSA test while simultaneously refusing to
have a digital rectal examination — is not a way to manage risk for
prostate cancer. On the other hand, not
getting a PSA test when you need one (for all sort of possible reasons)
is about as smart as not getting a vaccination against measles or
tetanus or a whole bunch of other deadly disorders. You may well not
need that vaccination. And you may well find you did not need the PSA
test (just as you may never need certain types of vaccination) … but
under the right conditions, any of these actions might help to save your
life.
The U.S. Preventive Services Task Force (USPSTF) issued a grade D recommendation that discouraged PSA-based screening for prostate cancer in October 2011, according to study background.
“The results raise concern that if this trend continues, more men may be diagnosed at a point when their disease
is advanced,” Barocas said. “Younger, healthier men with intermediate-
or high-risk disease would normally be candidates for aggressive local
therapy and they may not be receiving a timely diagnosis under this
policy.”
Researchers at Sanford-Burnham Medical Research Institute in Orlando are
working to more accurately diagnose prostate cancer starting with a set
of RNA molecules believed to regulate cell development.
Doctor Ranjan Perera, Associate Professor at Sanford-Burnham Medical Research Institute, said, "We were able to identify some of these RNAs being secreted in the urine of the prostate cancer patients." The team examined the urine and tissue samples of prostate cancer patients with those who did not have cancer and found the RNA levels were higher in those with cancer. Researchers say the RNAs are easily detected in urine.
"Our hope is that we can develop a urine test that would be a better biomarker for diagnosing prostate cancer," said Dr. Patel.
New screening that could be faster, more accurate, and end up saving even more lives. Professor Perera says the next step is to initiate a wide-scale clinical trial. He believes that the clinical study will be completed and a urine test will be developed and ready for use in three to five years.
Doctor Ranjan Perera, Associate Professor at Sanford-Burnham Medical Research Institute, said, "We were able to identify some of these RNAs being secreted in the urine of the prostate cancer patients." The team examined the urine and tissue samples of prostate cancer patients with those who did not have cancer and found the RNA levels were higher in those with cancer. Researchers say the RNAs are easily detected in urine.
"Our hope is that we can develop a urine test that would be a better biomarker for diagnosing prostate cancer," said Dr. Patel.
New screening that could be faster, more accurate, and end up saving even more lives. Professor Perera says the next step is to initiate a wide-scale clinical trial. He believes that the clinical study will be completed and a urine test will be developed and ready for use in three to five years.
Watching
'Genuine Change' in US
Prostate Cancer Management
In the years 2010-2013, the use of active surveillance for low-risk disease "increased sharply" to 40% of all cases, say investigators. The rate had languished at only about 10% in the preceding 20 years.
At the same time, use of androgen deprivation as a monotherapy "decreased sharply," they note, down to only 3.8% of intermediate-risk and 24% of high-risk prostate cancer cases. These percentages represent drops of about one third and one half from earlier periods.
Both trends are desirable because they represent strategies to avoid overtreatment and undertreatment, respectively.
In the years 2010-2013, the use of active surveillance for low-risk disease "increased sharply" to 40% of all cases, say investigators. The rate had languished at only about 10% in the preceding 20 years.
At the same time, use of androgen deprivation as a monotherapy "decreased sharply," they note, down to only 3.8% of intermediate-risk and 24% of high-risk prostate cancer cases. These percentages represent drops of about one third and one half from earlier periods.
Both trends are desirable because they represent strategies to avoid overtreatment and undertreatment, respectively.
More
men with prostate cancer are opting for surveillance | Reuters
There are several possible treatments for prostate cancer, including surgery and radiation. Some men - especially those who are older - may opt for active surveillance.
Men using active surveillance may undergo tests or biopsies to make sure the cancer isn't growing, the ACS says.
The approach helps avoid more aggressive treatments, which can carry the risk for complications such as incontinence and impotence.
There are several possible treatments for prostate cancer, including surgery and radiation. Some men - especially those who are older - may opt for active surveillance.
Men using active surveillance may undergo tests or biopsies to make sure the cancer isn't growing, the ACS says.
The approach helps avoid more aggressive treatments, which can carry the risk for complications such as incontinence and impotence.
Simply
observing men with very low-and low-risk prostate cancer very effective and
underused, UCLA researchers find - Medical News Today
"Ultimately, the decision-making process surrounding treatment for a man with localized prostate cancer must take an individualized approach. The risks and benefits of expectant management vis-a-vis active treatment should be reviewed with the patient in light of existing knowledge, potentially with the use of decision aids to help enable a truly shared decision-making process," the review states. "Active surveillance is a viable approach for most men with low-risk prostate cancer, and its broader adoption has the potential to stop the overtreatment of men with indolent lesions and redirect resources to men with more serious cancers."
"Ultimately, the decision-making process surrounding treatment for a man with localized prostate cancer must take an individualized approach. The risks and benefits of expectant management vis-a-vis active treatment should be reviewed with the patient in light of existing knowledge, potentially with the use of decision aids to help enable a truly shared decision-making process," the review states. "Active surveillance is a viable approach for most men with low-risk prostate cancer, and its broader adoption has the potential to stop the overtreatment of men with indolent lesions and redirect resources to men with more serious cancers."
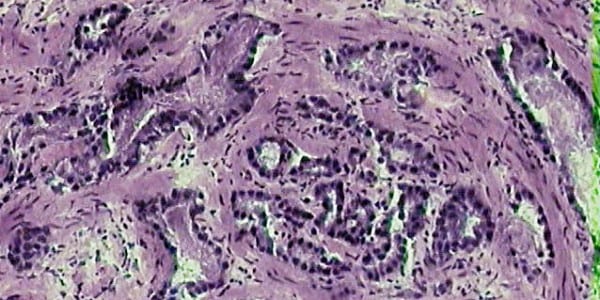
Biopsy/Pathology
 |
| Radical prostatectomy may trump radiotherapy in non-metastatic prostate cancer |
The inclusion of Gs=3+4 in patients suitable to AS does not enhance the risk of unfavourable disease after radical prostatectomy. Additional factors such as number of cores taken and the presence of ASAP should be considered in patients suitable for AS.
Access
: Improved detection of anterior fibromuscular stroma and transition zone
prostate cancer using biparametric and multiparametric MRI with MRI-targeted
biopsy and MRI-US fusion guidance : Prostate Cancer and Prostatic Diseases
MRI-targeted biopsies detected significantly more anteriorly located sPC compared with SBs in the repeat-biopsy setting. The more cost-efficient bpMRI was statistically not inferior to mpMRI in sPC detection in TZ/AFMS.
MRI-targeted biopsies detected significantly more anteriorly located sPC compared with SBs in the repeat-biopsy setting. The more cost-efficient bpMRI was statistically not inferior to mpMRI in sPC detection in TZ/AFMS.
Genomics
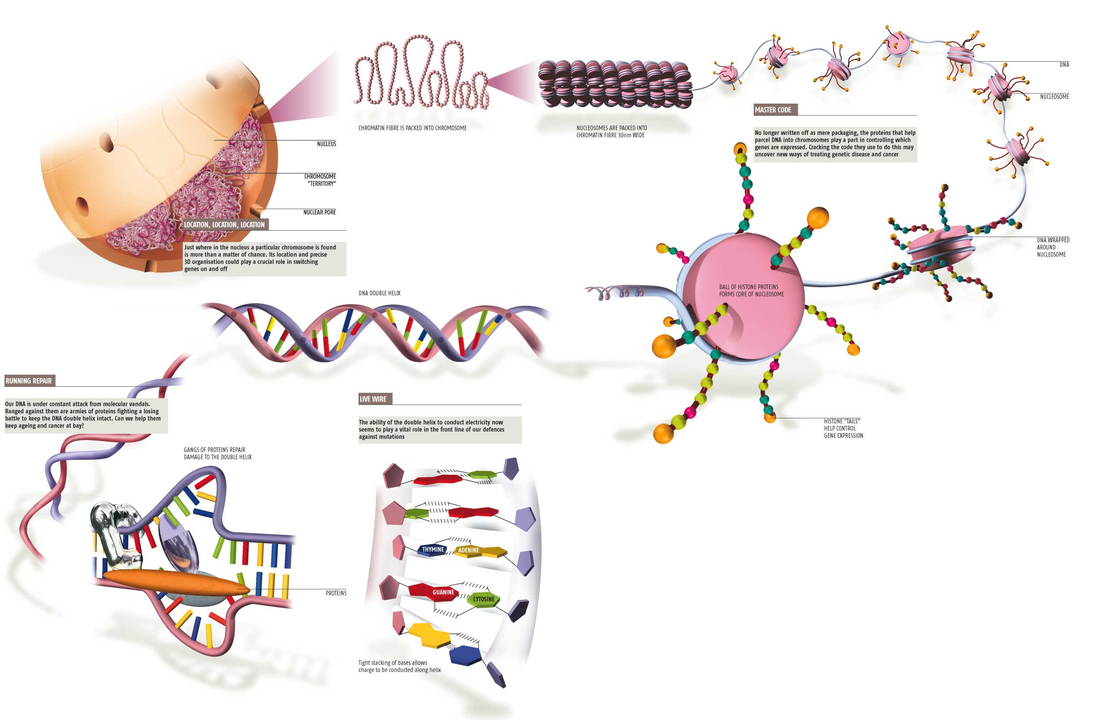 |
| Structural Organization of the Genome - Theory of Cancer Biology |
Prostate cancers are highly prevalent in the developed world, with inheritable risk contributing appreciably to tumour development. Genomic heterogeneity within individual prostate glands and between patients derives predominantly from structural variants and copy-number aberrations. Subtypes of prostate cancers are being delineated through the increasing use of next-generation sequencing, but these subtypes are yet to be used to guide the prognosis or therapeutic strategy. Herein, we review our current knowledge of the mutational landscape of human prostate cancer, describing what is known of the common mutations underpinning its development. We evaluate recurrent prostate-specific mutations prior to discussing the mutational events that are shared both in prostate cancer and across multiple cancer types. From these data, we construct a putative overview of the genomic evolution of human prostate cancer.
Study
Suggests 90% of Advanced Prostate Cancers May Have Anomaly that May Influence
Treatment - Cancer Therapy Advisor
Tt may soon be easier to treat metastatic castration-resistant prostate cancer (mCRPC) based on genetic anomalies. A new international study suggested it may be possible to link specific aberrations to response or resistance to specific treatments in 90% of cases.
Researchers from eight institutions in the United States and in Europe collaborated and sequenced the DNA and RNA of tumor biopsy samples from 150 men with mCRPC. They found that patients with mCRPC harbor genomic alterations in PIK3CA/B, RSPO, RAF, APC, B-catenin, and ZBTB16 and 23% harbor DNA repair pathway aberrations.1
Tt may soon be easier to treat metastatic castration-resistant prostate cancer (mCRPC) based on genetic anomalies. A new international study suggested it may be possible to link specific aberrations to response or resistance to specific treatments in 90% of cases.
Researchers from eight institutions in the United States and in Europe collaborated and sequenced the DNA and RNA of tumor biopsy samples from 150 men with mCRPC. They found that patients with mCRPC harbor genomic alterations in PIK3CA/B, RSPO, RAF, APC, B-catenin, and ZBTB16 and 23% harbor DNA repair pathway aberrations.1
New
Study Published on Cover of Urology Finds that Decipher® Prostate Cancer... --
SAN DIEGO, July 14, 2015 /PRNewswire/ --
The
Decipher test used in this study has been previously described in
multiple blinded independent validation studies in men at high risk of
recurrence at the time of prostatectomy. Researchers found that 60% of
the clinically high-risk men would be reclassified as low risk based on
the Decipher test and have only a 2.4% risk of metastasis at 5 years
after surgery. In addition, the 19% of the patients with the highest
risk based on Decipher had a nearly 10-fold higher risk of distant
metastases by 5 years. The test provided a more accurate and precise
estimate of a patient's risk of recurrence. Use of this test therefore
has the potential to assist clinicians to better direct utilization of
secondary therapy after surgery.
Researchers
Find Potential Achilles’ Heel for Prostate Cancer and B Cell Lymphoma |
Memorial Sloan Kettering Cancer Center
MicroRNAs are small molecules that regulate gene function. The laboratory of cancer biologist Andrea Ventura has found that one microRNA, miR-19, plays an important role in tumor cell growth in B cell lymphoma and prostate cancer. Blocking miR-19 seems to make cells resistant to these cancers while having no ill effects. The researchers also clarified the function of related microRNAs, which appear to play essential roles in embryonic development.
MicroRNAs are small molecules that regulate gene function. The laboratory of cancer biologist Andrea Ventura has found that one microRNA, miR-19, plays an important role in tumor cell growth in B cell lymphoma and prostate cancer. Blocking miR-19 seems to make cells resistant to these cancers while having no ill effects. The researchers also clarified the function of related microRNAs, which appear to play essential roles in embryonic development.
Access
: Which, when and why|[quest]| Rational use of tissue-based molecular testing
in localized prostate cancer : Prostate Cancer and Prostatic Diseases
An increased molecular understanding of localized prostate cancer and the improved ability for molecular testing of pathologic tissue has led to the development of multiple clinical assays. Here we review the relevant molecular biology of localized prostate cancer, currently available tissue-based tests and describe which is best supported for use in various clinical scenarios. Literature regarding testing of human prostate cancer tissue with Ki-67, PTEN (by immunohistochemistry (IHC) or fluroescence in situ hybridization (FISH)), ProMark, Prolaris, OncotypeDX Prostate and Decipher was reviewed to allow for generation of expert opinions. At diagnosis, evaluation of PTEN status, use of ProMark or OncotypeDX Prostate in men with Gleason 6 or 3+4=7 disease may help guide the use of active surveillance. For men with Gleason 7 or above disease considering watchful waiting, Ki-67 and Prolaris add independent prognostic information. For those men who have undergone prostatectomy and have adverse pathology, Decipher testing may aid in the decision to undergo adjuvant radiation. Newly available molecular tests bring opportunities to improve decision making for men with localized prostate cancer. A review of the currently available data suggests clinical scenarios for which each of these tests may have the greatest utility.
An increased molecular understanding of localized prostate cancer and the improved ability for molecular testing of pathologic tissue has led to the development of multiple clinical assays. Here we review the relevant molecular biology of localized prostate cancer, currently available tissue-based tests and describe which is best supported for use in various clinical scenarios. Literature regarding testing of human prostate cancer tissue with Ki-67, PTEN (by immunohistochemistry (IHC) or fluroescence in situ hybridization (FISH)), ProMark, Prolaris, OncotypeDX Prostate and Decipher was reviewed to allow for generation of expert opinions. At diagnosis, evaluation of PTEN status, use of ProMark or OncotypeDX Prostate in men with Gleason 6 or 3+4=7 disease may help guide the use of active surveillance. For men with Gleason 7 or above disease considering watchful waiting, Ki-67 and Prolaris add independent prognostic information. For those men who have undergone prostatectomy and have adverse pathology, Decipher testing may aid in the decision to undergo adjuvant radiation. Newly available molecular tests bring opportunities to improve decision making for men with localized prostate cancer. A review of the currently available data suggests clinical scenarios for which each of these tests may have the greatest utility.
Imaging
| New Imaging Approach to Map Prostate Cancer | BIRC |
Ward explains that the computer takes three different images of the prostate with different information, "and the idea is that this artificially intelligence system is going to automatically integrate and combine all of this information to produce a much simpler to read colour-coded road map for where the threatening areas of potential cancer are."
The
typical biopsy that doctors perform to check a man for prostate cancer is far
from a precise procedure, says the trial’s principle investigator Clare Tempany,
a radiologist and director of the National
Center for Image Guided Therapy at Brigham. Typically a physician
targets the prostate, which is the size of “a small peach or plum,” she says,
by placing a grid guide between the patient’s legs. Then the doctor inserts
needles through the skin and into each quadrant to get tissue samples.
“This is somewhat disparagingly called ‘the blind biopsy,’ ” says Tempany.
“There’s no lesion targeted, it’s just: ‘Let’s push a bunch of needles in and
see what we get.’ ”
These biopsies are sometimes aided by ultrasound
imaging, which requires inserting a ultrasound wand into the patient’s
rectum. Because ultrasound doesn’t provide clear enough images,
doctors aren’t able to make precision strikes with their needles, says
Tempany. They often end up taking 10 to 50 core samples, she says, and each
needle stick carries the risk of infection.
This clinical trial literally shows a better
way. Looking at real-time MRI images, the doctor can identify parts of the
prostate that look suspicious, and direct the robotic tool to those spots.
“In our procedure, a small little robot places the needle on the skin’s surface
and says, ‘This is the spot where you need to push, and in five or six centimeters
you’ll hit your target,’ ” Tempany explains. In the current trial the doctor
takes the actual step of inserting the needle, and typically takes
samples in just four locations. “It’s a smarter biopsy,” she says.
Treatment
Case
Studies Offer Window Into Evolving Prostate Cancer Paradigm
In recognition of this complexity, moderator Raoul S. Concepcion, MD, FACS, and colleagues took a case-based approach to explore the ways in which oncologists and urologists can employ newly acquired evidence to manage patients whom they encounter in their practices. The Peer Exchange session, entitled “Integrating Prostate Cancer Trial Findings Into Practice: A Case-Based Discussion,” incorporated four cases, two of which are presented here.
- See more at: http://www.onclive.com/publications/Oncology-live/2015/July-2015/case-studies-offer-window-into-evolving-prostate-cancer-paradigm#sthash.FozlFACb.dpuf
In
the ever-evolving treatment landscape in metastatic prostate cancer,
healthcare providers have more options that ever before. Although
guideline organizations have now incorporated the results of major
clinical trials into treatment paradigms, much controversy remains over
how best to sequence therapies, according to experts who participated in
a recent OncLive Peer Exchange.
In recognition of this complexity, moderator Raoul S. Concepcion, MD, FACS, and colleagues took a case-based approach to explore the ways in which oncologists and urologists can employ newly acquired evidence to manage patients whom they encounter in their practices. The Peer Exchange session, entitled “Integrating Prostate Cancer Trial Findings Into Practice: A Case-Based Discussion,” incorporated four cases, two of which are presented here.
- See more at: http://www.onclive.com/publications/Oncology-live/2015/July-2015/case-studies-offer-window-into-evolving-prostate-cancer-paradigm#sthash.FozlFACb.dpuf
In the ever-evolving treatment landscape in metastatic prostate cancer, healthcare providers have more options that ever before. Although guideline organizations have now incorporated the results of major clinical trials into treatment paradigms, much controversy remains over how best to sequence therapies, according to experts who participated in a recent OncLive Peer Exchange.In recognition of this complexity, moderator Raoul S. Concepcion, MD, FACS, and colleagues took a case-based approach to explore the ways in which oncologists and urologists can employ newly acquired evidence to manage patients whom they encounter in their practices. The Peer Exchange session, entitled “Integrating Prostate Cancer Trial Findings Into Practice: A Case-Based Discussion,” incorporated four cases, two of which are presented here.
- See more at: http://www.onclive.com/publications/Oncology-live/2015/July-2015/case-studies-offer-window-into-evolving-prostate-cancer-paradigm#sthash.FozlFACb.dpuf
In recognition of this complexity, moderator Raoul S. Concepcion, MD, FACS, and colleagues took a case-based approach to explore the ways in which oncologists and urologists can employ newly acquired evidence to manage patients whom they encounter in their practices. The Peer Exchange session, entitled “Integrating Prostate Cancer Trial Findings Into Practice: A Case-Based Discussion,” incorporated four cases, two of which are presented here.
- See more at: http://www.onclive.com/publications/Oncology-live/2015/July-2015/case-studies-offer-window-into-evolving-prostate-cancer-paradigm#sthash.FozlFACb.dpuf
Radiation
Pioneering
treatment for prostate cancer sufferers (From The Northern Echo)
Specialists at Middlesbrough's James Cook University Hospital will be able to use radioactive radium 223 to treat prostate cancer patients for the first time.
The radium is used to treat prostate cancer which has spread to the bones and specifically targets tumours with less pain and fewer side effects.
Radiation
therapy may improve survival even when PSA ≥ 75 ml/ml | THE "NEW"
PROSTATE CANCER INFOLINKSpecialists at Middlesbrough's James Cook University Hospital will be able to use radioactive radium 223 to treat prostate cancer patients for the first time.
The radium is used to treat prostate cancer which has spread to the bones and specifically targets tumours with less pain and fewer side effects.
Sometimes, when patients originally present with very high PSA levels, a negative bone scan, and a negative CT scan, they are put on permanent androgen deprivation therapy (ADT) because the doctor just assumes it is micrometastatic. A closer look at the data demonstrates that an attempt at curative radiation may improve outcomes.
Access
: Primary radiotherapy vs conservative management for localized prostate
cancer|[mdash]|a population-based study : Prostate Cancer and Prostatic
Diseases
Among men >65 years of age, the benefit of primary radiotherapy for localized disease is largely confined to patients with high-risk prostate cancer (Gleason scores 7–10).
Among men >65 years of age, the benefit of primary radiotherapy for localized disease is largely confined to patients with high-risk prostate cancer (Gleason scores 7–10).
Prostate
cancer: Radiotherapy is effective in old men with high-risk cancer : Nature
Reviews Urology : Nature Publishing Group
In a population-based study of 57,749 patients with prostate cancer, the effectiveness of primary radiotherapy versus conservative management was investigated by comparing patient outcomes in geographical areas with high, versus low radiotherapy use. In older patients (>65 years of age), those in high radiotherapy use areas had small, but significant…
In a population-based study of 57,749 patients with prostate cancer, the effectiveness of primary radiotherapy versus conservative management was investigated by comparing patient outcomes in geographical areas with high, versus low radiotherapy use. In older patients (>65 years of age), those in high radiotherapy use areas had small, but significant…
Low
utilization of immediate and delayed postoperative radiation for prostate
cancer with adverse pathologic features - Beyond the Abstract
immediate radiotherapy is still being underutilized after prostatectomy, and this underutilization does not appear to be explained entirely by the use of delayed radiotherapy, which is also low. Urologists should discuss the risks, benefits, and evidence behind immediate vs. delayed radiotherapy with their patients. For those patients who are considering postoperative radiotherapy, referral to a radiation oncologist may be beneficial.
immediate radiotherapy is still being underutilized after prostatectomy, and this underutilization does not appear to be explained entirely by the use of delayed radiotherapy, which is also low. Urologists should discuss the risks, benefits, and evidence behind immediate vs. delayed radiotherapy with their patients. For those patients who are considering postoperative radiotherapy, referral to a radiation oncologist may be beneficial.
Increased
radiation offers no survival benefit for patients with low-risk prostate cancer
Increased radiation dose is associated with higher survival rates in men with medium- and high-risk prostate cancer, but not men with low-risk prostate cancer, according to a new study from Penn Medicine published this week in JAMA Oncology. Already-high survival rates for men with low-risk prostate cancer were unaffected by higher radiation dosages compared to lower radiation dosages.
Increased radiation dose is associated with higher survival rates in men with medium- and high-risk prostate cancer, but not men with low-risk prostate cancer, according to a new study from Penn Medicine published this week in JAMA Oncology. Already-high survival rates for men with low-risk prostate cancer were unaffected by higher radiation dosages compared to lower radiation dosages.
Hormone Therapy
Statin
Therapy May Help Delay Prostate Cancer Progression in Men Receiving ADT -
Cancer Therapy Advisor
Taking a statin while undergoing androgen deprivation therapy (ADT) for prostate cancer appears to pay off when it comes to delaying disease progression, according to researchers at the Dana-Farber Cancer Institute. They analyzed data on 926 men with prostate cancer receiving ADT and found that time to progression (TTP) was significantly delayed if the men were taking a statin.
Taking a statin while undergoing androgen deprivation therapy (ADT) for prostate cancer appears to pay off when it comes to delaying disease progression, according to researchers at the Dana-Farber Cancer Institute. They analyzed data on 926 men with prostate cancer receiving ADT and found that time to progression (TTP) was significantly delayed if the men were taking a statin.
Androgen
deprivation of prostate cancer: Leading to a therapeutic dead end.
In this review, we describe molecular alterations in tumor cells during ADT, which lead to deregulation of different signaling pathways and castration-resistance, and how they might interfere with the clinical outcome of different second-line therapeutics. A recent breakthrough finding that early chemotherapy is associated with a significant survival benefit in metastatic hormone-sensitive disease highlights the fact that there is time for a fundamental paradigm shift in the treatment of advanced prostate cancer. Therapeutic intervention seems to be indicated before a castration-resistant stage is reached to improve therapeutic outcome and to reduce undesirable side effects.
In this review, we describe molecular alterations in tumor cells during ADT, which lead to deregulation of different signaling pathways and castration-resistance, and how they might interfere with the clinical outcome of different second-line therapeutics. A recent breakthrough finding that early chemotherapy is associated with a significant survival benefit in metastatic hormone-sensitive disease highlights the fact that there is time for a fundamental paradigm shift in the treatment of advanced prostate cancer. Therapeutic intervention seems to be indicated before a castration-resistant stage is reached to improve therapeutic outcome and to reduce undesirable side effects.
Chemo
Predicting
response to chemotherapy for prostate cancer and other stories . . . | The BMJ
A new study shows that the measurement of androgen receptor splice variant 7 (AR-V7) in circulating tumour cells can predict which men with castration resistant prostate cancer are most likely to respond to treatment with chemotherapy rather than enzalutamide or abiraterone (JAMA Oncology 2015, doi:10.1001/jamaoncol.2015.1341).
Detection of AR-V7 in CTCs from men with metastatic CRPC is not associated with primary resistance to taxane chemotherapy. In AR-V7–positive men, taxanes appear to be more efficacious than enzalutamide or abiraterone therapy, whereas in AR-V7–negative men, taxanes and enzalutamide or abiraterone may have comparable efficacy. Circulating tumor cell–based AR-V7 detection may serve as a treatment selection biomarker in CRPC.
A new study shows that the measurement of androgen receptor splice variant 7 (AR-V7) in circulating tumour cells can predict which men with castration resistant prostate cancer are most likely to respond to treatment with chemotherapy rather than enzalutamide or abiraterone (JAMA Oncology 2015, doi:10.1001/jamaoncol.2015.1341).
Detection of AR-V7 in CTCs from men with metastatic CRPC is not associated with primary resistance to taxane chemotherapy. In AR-V7–positive men, taxanes appear to be more efficacious than enzalutamide or abiraterone therapy, whereas in AR-V7–negative men, taxanes and enzalutamide or abiraterone may have comparable efficacy. Circulating tumor cell–based AR-V7 detection may serve as a treatment selection biomarker in CRPC.
Advanced - Recurrent
A
bird's eye view of advanced prostate cancer
An estimated 220,000 American men are diagnosed with prostate cancer each year, with 30,000 expected to die of it this year. While androgen deprivation therapy (ADT) is initially effective against metastatic disease, most men develop tumors that ultimately become resistant to ADT, including the most recent ADT regimen (abiraterone acetate and enzalutamide). This condition is known as metastatic castration-resistant prostate cancer (mCRPC). While many studies have cataloged somatic alterations in primary prostate cancers, genomic studies of mCRPC have been limited to either autopsy samples or preclinical models. To address the gap in our understanding of mCRPC, an international and multi-institutional consortium that included Fred Hutch investigators and benefitted from key contributions from Dr. Pete Nelson’s Laboratory (Human Biology, Clinical Research and Public Health Sciences Divisions), sequenced the DNA and RNA from biopsies of bone or soft tissue metastases prospectively from 150 mCRPC affected individuals. This work was recently published in the journal Cell.
An estimated 220,000 American men are diagnosed with prostate cancer each year, with 30,000 expected to die of it this year. While androgen deprivation therapy (ADT) is initially effective against metastatic disease, most men develop tumors that ultimately become resistant to ADT, including the most recent ADT regimen (abiraterone acetate and enzalutamide). This condition is known as metastatic castration-resistant prostate cancer (mCRPC). While many studies have cataloged somatic alterations in primary prostate cancers, genomic studies of mCRPC have been limited to either autopsy samples or preclinical models. To address the gap in our understanding of mCRPC, an international and multi-institutional consortium that included Fred Hutch investigators and benefitted from key contributions from Dr. Pete Nelson’s Laboratory (Human Biology, Clinical Research and Public Health Sciences Divisions), sequenced the DNA and RNA from biopsies of bone or soft tissue metastases prospectively from 150 mCRPC affected individuals. This work was recently published in the journal Cell.
Regional
hyperthermia and moderately dose-escalated salvage radiotherapy for recurrent
prostate cancer. Protocol of a phase II trial
Current studies on salvage radiotherapy (sRT) investigate timing, dose-escalation and anti-hormonal treatment (ADT) for recurrent prostate cancer. These approaches could either be limited by radiation-related susceptibility of the anastomosis or by suspected side-effects of long-term ADT.
A phase II protocol was developed to investigate the benefit and tolerability of regional hyperthermia with moderately dose-escalated radiotherapy.
Current studies on salvage radiotherapy (sRT) investigate timing, dose-escalation and anti-hormonal treatment (ADT) for recurrent prostate cancer. These approaches could either be limited by radiation-related susceptibility of the anastomosis or by suspected side-effects of long-term ADT.
A phase II protocol was developed to investigate the benefit and tolerability of regional hyperthermia with moderately dose-escalated radiotherapy.

No comments:
Post a Comment